by Elana Sitnik
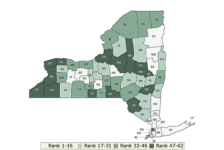
Across New York State, rural communities face a critical shortage of primary care physicians, hindering access to essential healthcare. Although New York State trains more medical residents than any other state, there are very few residency programs located in rural communities. A 2019 report by the Primary Care Development Corporation highlights the dwindling number of primary care physicians in rural communities, leaving rural New Yorkers with longer wait times for medical appointments and limited access to life-prolonging and cost-saving preventative care. (1,2)
The solution lies not only in attracting doctors to these areas but also in developing a sustainable source of future physicians who understand the unique needs of these underserved rural communities. Smaller residency programs, which are often located in rural communities struggling with primary care access, can play a vital role in improving access to healthcare in rural communities. Research shows that doctors who train in programs serving rural populations are far more likely to choose to practice in those areas after residency.
Dr. Caleb Atkins is one of only two second-year family medicine residents at Samaritan Medical Center in Watertown, NY. A native of Jefferson County, Dr. Atkins grew up just 20 miles away in the small town of Carthage, NY. His interest in practicing rural family medicine stems from witnessing his parents’ poor health outcomes due to limited healthcare access during his upbringing. Dr. Atkins appreciates his training environment, stating, “Training in the Family Medicine Residency at Samaritan Medical Center provides me with unfettered access to a wide variety of diseases in a close-knit residency setting.” He describes his medical training as indispensable. However, he expresses concern about the future of programs like his, noting, “The program’s inability to secure more federal funding for expansion is worrisome.” He emphasizes, “Without additional doctors being trained in my area, healthcare outcomes will continue to suffer.”
By strengthening Medicaid funding for these rural and safety-net hospital residency programs, the New York State legislature can solve three of our state’s public health challenges in just one move: the physician shortage, increasing access to care for rural communities, and keeping physicians who train in New York in the state once their training is complete. Increased funding would allow these programs to expand residency slots, directly addressing the physician shortage in New York. Additionally, more residency positions in rural settings will translate into a larger pool of physicians qualified to address the specific needs of rural communities, and studies show that increased exposure to rural healthcare during residency has potential to encourage graduates to consider practicing in rural areas (3).
Dr. Jocelyn Young, Designated Institutional Official at Chenango Memorial Hospital is leading the creation of a rural family medicine residency program in the community of Norwich, in Central New York. She highlights that recruitment of primary care physicians to the small community is very challenging. CMH has embarked on creating a residency program that seeks to recruit, train, and retain the next generation of family physicians who will serve the area. “Through creating a program that allows residents to train in the environment that we hope they will practice in, this rural farming community will be served by dedicated family physicians for generations to come.” One of the challenges in creating a new residency program is finding the financial resources to offset the cost of creating and running an excellent quality residency program. As a sole community hospital, CMH is limited in access to Medicare funding for residency training. “Increased medicaid funding within the state that is focused on institutions that are training rural primary care physicians would ease the burden being shouldered by small hospitals.” The team at CMH is boldly striding forward despite these challenges and Dr. Young plans to continue advocating to increase NYS Medicaid funding for rural residencies and their hospitals.
In essence, investing in rural residency programs isn’t just about creating more doctors – it’s about creating doctors who are invested in serving the very communities that need them most. Doctors, hospital administrators, and lawmakers all have a stake in ensuring equitable access to healthcare across New York State. By prioritizing funding for rural residency programs, we can cultivate a future generation of physicians dedicated to these underserved communities. This isn’t just about healthcare, it’s about fostering healthy and thriving communities throughout our state. Let’s write the prescription for a healthier rural New York by investing in the doctors who will serve these communities for years to come.
- Rural access to primary care in New York State: 2019 Report. https://www.pcdc.org/wp-content/uploads/Resources/Rural-Access-to-Primary-Care-in-New-York-State-_-2019-Report.pdf
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2690145/
- Recipe for more rural physicians: More exposure in residency training. American Medical Association. Published September 27, 2022. Accessed February 23, 2024.https://www.ama-assn.org/medical-residents/transition-resident-attending/recipe-more-rural-physicians-more-exposure